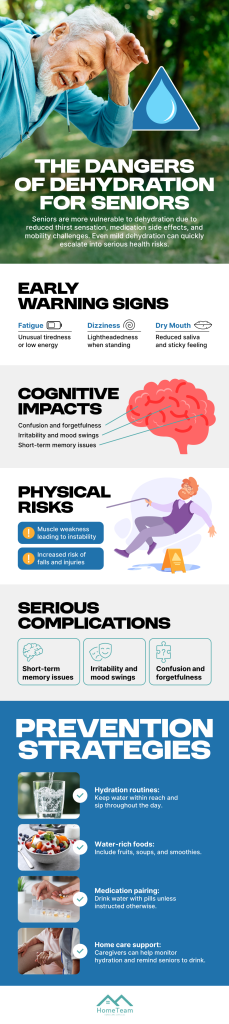
Dehydration is a health concern at any age, but older adults face higher risks because the body becomes less efficient at conserving water. Many seniors also have weaker thirst cues, meaning they may not feel thirsty until they are already dehydrated. What starts as mild fluid loss can quickly progress into a serious condition. Recognizing why dehydration occurs and how it affects the body is an important step in keeping aging loved ones safe.
Why Seniors Are More Vulnerable
As the body ages, natural changes occur that influence hydration. Kidney function gradually declines, which affects the body’s ability to maintain fluid balance. Seniors may drink less because of mobility challenges, fear of frequent bathroom trips, or medications that increase fluid loss. Chronic illnesses such as diabetes, heart disease, and memory impairments can also make regular drinking more difficult.
Many older adults rely on routines, and if hydration is not part of those routines, it may slip through the cracks. Even small amounts of lost fluid add up, especially during warm weather, exercise, or illness. Caregivers and family members should watch for reduced fluid intake in daily activities, as early intervention can prevent more serious issues.
How Dehydration Impacts Physical Health
Dehydration affects nearly every system in the body. When fluid levels drop, blood becomes more concentrated, making it harder for the heart to pump efficiently. Seniors may experience dizziness, headaches, or rapid heart rate as the body struggles to compensate. These symptoms increase the risk of falls, one of the most significant hazards for older adults.
Digestion also slows when fluids are low. Constipation becomes more common, and medications may not absorb properly. Urinary tract infections are more likely because dehydration reduces urine output. For seniors with chronic conditions, even mild dehydration can worsen symptoms.
Cognitive and Emotional Effects of Dehydration
Proper hydration supports the brain as much as the body. When seniors become dehydrated, confusion, fatigue, irritability, and poor concentration often appear. These symptoms can be mistaken for dementia or mood changes, leading families to overlook dehydration as the underlying cause. In more severe cases, dehydration may contribute to delirium, which requires medical attention.
Because the brain relies heavily on electrolyte balance, even small shifts caused by low fluid levels can impact communication, memory, and decision making. Keeping seniors hydrated supports clearer thinking and reduces the likelihood of avoidable medical concerns.
Practical Ways to Encourage Consistent Hydration
Hydration strategies work best when they fit easily into a senior’s routine. Offering water at regular intervals rather than relying on thirst helps maintain steady intake. Some older adults enjoy flavored water, herbal teas, broth, or fruits with high water content such as oranges or watermelon. These small adjustments provide hydration without feeling overwhelming.
Using lightweight cups, keeping drinks within reach, and setting reminders throughout the day can also help. For seniors who receive structured in-home support, some CDS providers assist with hydration tracking as part of daily care routines. Families can ask health professionals or care teams for customized suggestions based on specific medical needs.
Recognizing Early Warning Signs
Early signs of dehydration may include dry mouth, fatigue, dark urine, or reduced urination. Seniors may also seem less steady or more forgetful than usual. When these symptoms appear, offering fluids promptly and increasing water rich foods can help. If symptoms escalate to confusion, rapid heartbeat, fainting, or extreme weakness, medical help is needed.
Dehydration is preventable, and small habits can make a meaningful difference. With attentive care, thoughtful planning, and consistent reminders, seniors can maintain healthier fluid levels and enjoy greater stability and well-being as they age. Look over the infographic below for more information.